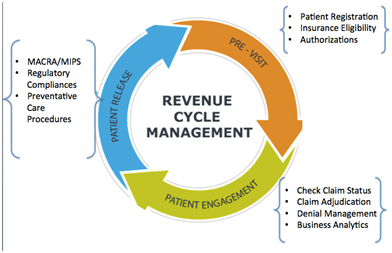
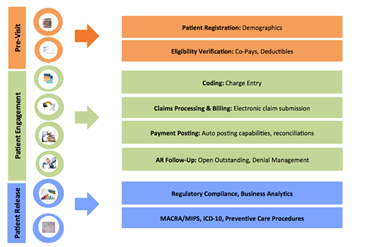
MMMBS, Inc. Revenue Cycle Management services encompass the entire life cycle of the patient account from creation to payment. Services included with the flat-rate Billing Service include:
- Billing Software & Practice Management Software set-up, and Database & Practice Set-up included (at no cost)
- Credentialing (at no cost)
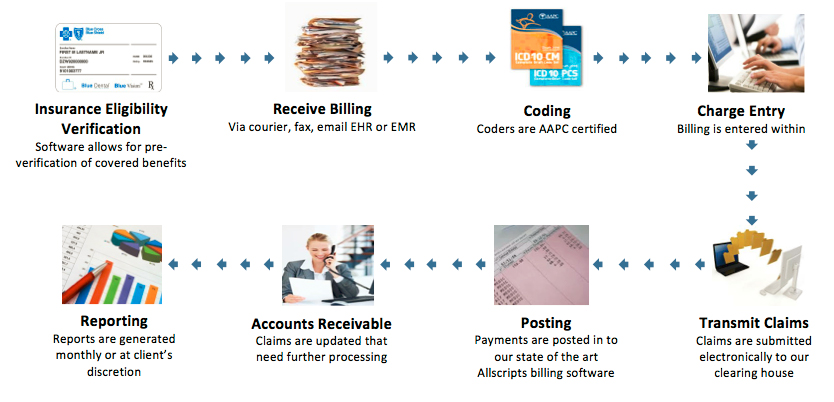
- Insurance Eligibility Verification using our state-of-the-art software that checks benefit information including co-pays and deductibles in real-time from any computer with wi-fi access (at no cost)
- All Services related to billing and coding (see medical billing workflow below)
- Review & update of fee schedules
- Updates on Industry changes, regulatory compliances, & monthly financial reporting
Our billing is designed to increase your reimbursement. Key features include:
- AAPC (American Academy of Professional Coders) certified coders to provide physicians with accurate billing & coding policy
- 48 hour turn-around-time for charge entry after MMMBS, Inc. receives your billing
- Utilization of AllScripts Billing software
- An Industry leading 97.8% average reimbursement rate on all insurance claims submitted (most companies typically average 70-75% reimbursement)
Combining MMMBS, Inc. certification and state-of-the-art software, most of our clients find their income substantially increase due to the accuracy of our coding and the quality of our follow-up services!
Billing Process
As part of the billing service and MMMBS’s Client Management Relationship Approach, we assign each client with 3 direct contact representatives:
1) Billing/Coding Specialist
- Focus on proper ICD-10, CPT, and HCPCS coding
- Review medical record documentation to validate & ensure proper charge capture
- Report insufficient documentation issues
- Report over-coding/undercoding issues
- Work with Reimbursement Specialists & Account Managers to ensure minimum claim denials
2) Reimbursement Specialist
- Focus on payment posting, denials management, unpaid claims
- Reconcile/record batch payments from insurance payers
- Responsible for managing 1°, 2°, 3° claims ageing reports
- Communicate directly with insurance payers to resolve claims issue
- Create & file appeals as necessary
- Effectively communicate coding/billing issues which are causing denials to both account managers & billing specialist
3) Account Manger
- Responsible for coordination and quality assurance of all aspects of customer’s revenue cycle
- Provides customer service- main point of contact
- Understands & communicates coding/billing/compliance regulations
- Manages patient invoicing and collections
- Works with other 2 reps to maximize overall account efficiency
You will also work closely with a credentialing specialist during the implementation phase of service.

